Atkins Diet, South Beach, the Whole 30, Paleo and now Keto? What’s this all about? What does it mean and how can you educate your clients about the potential benefits and barriers?
First, let’s take a look at the keywords and their definitions.
Ketogenic
“Related to the excessive amounts of ketone bodies in the body tissues and fluids as a result of incompletely metabolized fatty acid or amino acid breakdown” (Porcari, Byrant, & Comana, 2015).
Ketone body
“Any of the acidic products of lipid metabolism that may accumulate in blood” (Thibodeau & Patton, 2012).
Ketoacidosis
“A metabolic state marked by the accumulation of ketone bodies (ketones) attributed to incompletely metabolized fatty acids or amino acids on account of inadequate amounts of available carbohydrates; results in lowering blood pH which can be potentially harmful and presence of ketones (acetone) on a person’s breath” (Porcari et al., 2015).
This is known as diabetic ketoacidosis in individuals with diabetes.
Watch the NFPT Live Episode on the Ketogenic Diet
Ketogenic Diet Composition
At the most simplified level, ketones build up when the body is using fats and/or amino acids (instead of carbohydrates) as fuel. We know carbohydrates are the body’s “go to” or preferred energy source (even the brain runs off glucose). However, when the amount of available carbohydrates is low, the body turns to fats and protein to metabolize and create new sources of sugar.
This alternative a survival mechanism.
A typical ketogenic diet is characterized by the following (or similar) macronutrient distribution:
- 5-10% carbohydrates (very low intake)
- 10-20% protein (moderate intake)
- 70-80% fat (very high intake)
Let’s do the math. On a 2,000-calorie diet, the daily caloric distribution would look as follows.
- 100-200 calories from carbohydrates (approximately 25-50 grams)
- 200-400 calories from protein (approximately 50-100 grams)
- 1,400-1,600 calories from fat (approximately 156-178 grams)
Eating this type of macronutrient pattern forces the body to deplete stored carbohydrates and turn to alternative fuel sources – fats (this includes body fat, as well) and proteins.
This reaction takes anywhere from three to four days.
As the body is being depleted, individuals often report experiencing a “keto flu” with symptoms of achiness, fatigue, weakness, irritability, reduced libido, and constipation (from a lack of fibrous foods such as grains and fruits). In short, the first week on a keto diet isn’t pleasant or tranquil.
You are basically forcing the body to search for other sources of energy (Paoli, Rubini, Volek, & Grimaldi, 2013).
What do you eat on a Keto Diet?
In short, an abundance of good fats (nuts, seeds, avocado oil, olive oil), lean proteins (salmon, grass-fed beef, organic/non-GMO poultry, fermented dairy), and non-starchy veggies. The main goal is to cut out all processed carbohydrates, sugar (including intrinsic sugars found in fruits and grains that cause an “insulin spike”).
Keep in mind, the “not so helpful gut bacteria” thrive on processed food and sugar, so cutting these items out of the daily diet plan helps restore gut health and good bacteria. Many keto-friendly foods are also anti-inflammatory and have been shown to be beneficial for those with certain digestive issues.
Low-carb diets go awry when individuals do not consume “clean” sources of foods and consume carelessly foods high in saturated fat. Not all fats are created equal and the keto diet doesn’t promote eating a pound of bacon a day or a 32-ounce prime rib steak three times a week. The keto diet aims to encourage quality intake of mostly fats and moderate protein.
A ketogenic diet is not synonymous with a high protein diet.
What does the research say?
Before you write off the ketogenic diet as another “fad” in the great list of crazy restrictive dieting approaches, let’s examine some of the established and emerging research findings.
A ketogenic diet is a low carb/ high-fat diet. Its basic premise of keeping carbs low is similar to other “low carb” diet trends we’ve seen in the past. Low carb diets, surprisingly enough, have existed since the 1920s and were once used to treat epilepsy although it’s mechanism of action remains a mystery. In later decades, the low carb craze became a way to “treat” obesity (Paoli et al., 2013). Still, there are other purported health benefits and areas of developing research that raise some interesting questions about disease treatment and prevention.
Research has indicated that a ketogenic diet has benefits for weight loss and type II diabetes. Other studies have examined benefits for acne, cancer prevention, polycystic ovary syndrome (PCOS), and treatment for neurodegenerative diseases.
Weight Loss
There is a thermogenic effect of food. This is the energy that it costs the body to digest and metabolize nutrients. It costs more energy to metabolize fats and protein than it does to metabolize carbohydrates, so the body is likely burning more calories. Second, this type of diet has appetite suppressing qualities (Gibson, Seimon, Lee, Ayre, Franklin, Markovic, Caterson, & Sainsbury, 2015). This ultimately leads to consuming fewer calories than are burned and a more favorable body composition.
Diabetes treatment
In restricting the number of carbohydrates consumed, insulin sensitivity is restored. In turn, this will positively impact A1c levels and encourage a return to healthy blood sugar levels (Gibas & Gibas, 2017).
Acne
This area of research is developing and interesting. There is a belief among researchers that certain foods stimulate pathways that ultimately lead to the development of acne (Paoli et al., 2013). Further trials are needed to draw conclusive results about how these pathways work and influence acne.
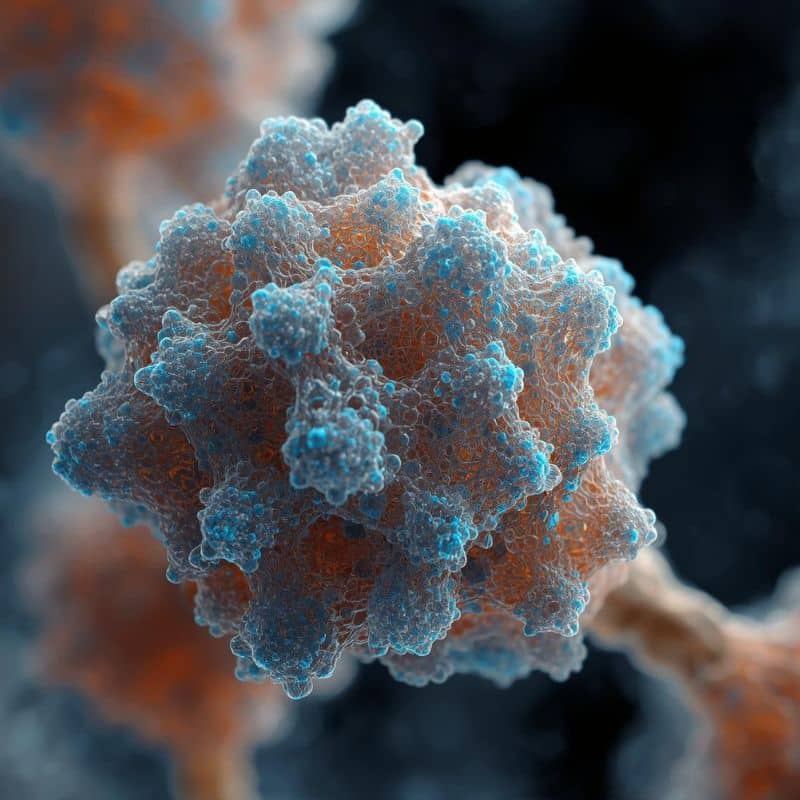
Cancer
Tumor cells are glucose lovers and they thrive and grow in its presence. The hope and theory is that if we starve the tumor food supply by depleting glycogen, we starve the tumors themselves (Paoli et al., 2013). The question remains if the human body can adapt to other means of energy and substrate utilization, can other cells such as cancer do the same?
Polycystic Ovary Syndrome (PCOS)
Hyperinsulinemia and insulin resistance are quite commonly seen in women who also suffer from PCOS. Again, one of the thoughts here is to restore insulin sensitivity and positively impact the condition (Paoli et al., 2013).
Neurodegenerative Diseases
This may be the most interesting area of study with regard to ketogenic diets as therapeutic approaches. There appears to be a neuroprotective effect of ketogenic diets in many of these types of diseases.
According to Paoli et al. (2013), a common characteristic of neurological diseases is a disruption or defect in “cellular energy utilization”, which may explain why forcing the body to choose a different source for energy can positively impact this category of afflictions. However, this area of study is still new and many questions are left to explore. Nonetheless, the preliminary information is promising.
Is ketogenic safe for everyone?
No. This is not a diet that just anyone should adopt nor one that just any health and fitness professional should recommend. It is outside the scope of practice for anyone but a medical doctor or licensed registered dietitian to recommend and supervise.
If your clients ask about the diet, do what you do best. Educate them on what the diet is and how it works, but consistently advise clients to seek the counsel of a qualified professional to help them determine if the ketogenic approach is appropriate.
It is not necessary to follow a ketogenic diet indefinitely. Many find these types of diets impossible to sustain and that’s ok. The most significant priority is helping your clients shape and develop sustainable healthy eating styles that they will enjoy consuming. Remember – diet, like exercise, is not one-size-fits-all. Treat each client as they are – an individual with a unique set of needs and goals.
References
Gibas, M.K., & Gibas, K.J. (2017). Induced and controlled dietary ketosis as a regulator of obesity and metabolic syndrome pathologies. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 11, S385-390. doi: 10.1016/j.dsx.2017.03.022
Gibson, A. A., Seimon, R. V., Lee, C. M. Y., Ayre, J., Franklin, J., Markovic, T. P., Caterson, I. D. and Sainsbury, A. (2015), Do ketogenic diets really suppress appetite? A systematic review and meta-analysis. Obesity Rev, 16, 64–76. doi:10.1111/obr.12230
Porcari, J., Bryant, C., & Comana, F. (2015). Exercise Physiology. Philadelphia, PA: FA Davis.
Thibideau, G., & Patton, K. (2012). Structure & Function of the Body. St. Louis, MO: Elsevier
Paoli, A., Rubini, A., Volek, J. S., & Grimaldi, K. A. (2013). Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. European Journal of Clinical Nutrition, 67(8), 789–796. doi.org/10.1038/ejcn.2013.116