Shin splints, or as it is clinically referred to, medial tibial stress syndrome, affects one percent of the population per year, but what is it? To better understand this, we must first look at the basic anatomy of what is referred to as the crural region of our bodies. This region consists of the bones, muscles, intraosseous membranes, and other tissues distal to the knee. Specifically of concern is the tibia bone and the tibialis anterior muscle.
The Lower Leg Anatomy
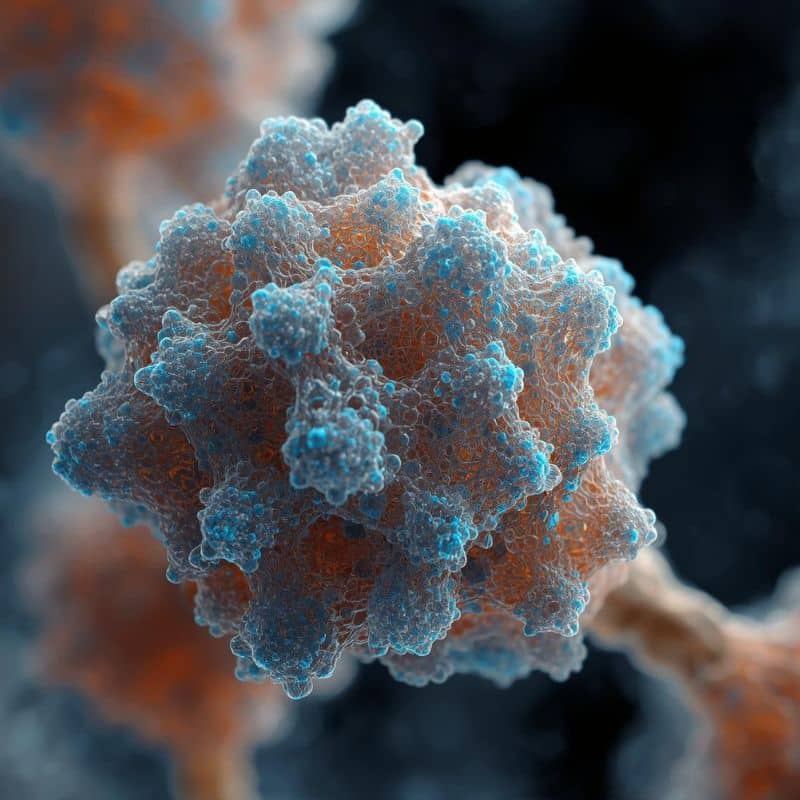
The tibia bone consists of essentially three articulations between the femur (at the knee), with the fibula (just inferior to the knee) and the foot (at the ankle). This bone also has multiple layers, including the periosteum which will be our primary focus. The periosteum is simply the outer lining of the bone that consists of multiple cell types to include osteocytes, osteoclasts, osteogenic, and osteoblasts. Each of these cells has a special function, but again for our purposes, we will narrow down to the two most important cells for describing the pathology of this ailment.
The osteoclasts and the osteoblasts are involved at a cellular level in the reabsorption of unneeded or damaged bone, and the formation of new bone, respectively.
This process is highlighted to show that our bones are not simply static entities like rocks, as some might imagine, but a multicellular tissue that is very dynamic in nature!
The muscles of importance in understanding medial tibial stress syndrome are the soleus and the anterior tibialis. The soleus is a deep, powerful muscle on the posterior of the leg. It originates just inferior to the knee and inserts in the cuneiform bones of the foot. Similarly, the tibialis anterior originates just inferior to the knee as well and inserts into the medial cuneiform bones of the foot. These muscles are antagonistic, (meaning, they perform opposing actions) but both are extremely important in our ability to run and walk.
The Pathology of Shin Splints
Now that we have a basic understanding even down to the cellular level of this region’s anatomy, let’s talk about medial tibial stress syndrome.
Simply put, shin splints is a catch-all diagnosis for lower leg pain in the anterior crural region. However, for the sake of specificity, we shall refer to the diagnosis more specifically as medial tibial stress syndrome. Medial tibial stress syndrome is caused by repetitive impact exercise with the absence of stress fractures. The increased stress from repetitive impacts results in microtears in the muscle and micro cortical fractures of the bone.
Accompanying this is also often periostitis, which is an inflammation of the external layer of cells in our bones that we previously mentioned- the periosteum. There has been some debate as to whether the periostitis causes the microfractures or the microfractures cause the periostitis.
Regardless, there are multiple forces acting on the tibia and its accompanying muscles in running, which is the most common cause of shin splints. There is an impact with the ground, which travels up through the body each time, as well as a slew of tension forces from each of the muscles that occur as they contract in order to lift our feet and provide stabilization during the act of running. Similarly, this can be caused by other repetitive impact exercises.
What Fit Pros Can Do
While we are not entirely clear on the pathophysiology of this injury, there may be some things that can be done to help limit the risk or severity of the injury!
1. Warm-Up
Warming up/stretching will help relieve some of the additional tension in these muscles. The goal here is to stretch them out and relax them some prior to repetitive impact exercises. This reduction in tension is theoretically also a reduction in force exerted on the bone by your own musculature. While recent research indicates that static stretching prior to activity results in lowered performance (due to force reduction output), when a muscle is short and overactive, this is not a bad idea. Starting with myofascial release will help release adhesions and allow for a more effective stretch.
2. Ice
There is some controversy over whether ice helps prevent or heal shin splints, but hear me out here. Since the science is still out on whether the periostitis or the micro cortical fractures occur first, there is some chance that the ice may help in the reduction in inflammation post-running sessions. By reducing this inflammation of the periosteum, there may be a reduction in pressure that is causing microfractures in the outer layer of the bone. Similarly, it may help relieve some of the soreness in the microtears of the tibialis anterior.
3. Strengthen
There is some research that suggests strengthening the muscles involved will help increase stability and reduce the impact on the bone from impact exercises. Other research suggests that strengthening the hip abductors may aid in reduction of shin splints by increasing the stability further up the kinetic chain while running.
But there’s another point that needs to be made about this: the tibia, soleus, and tibialis anterior will all strengthen themselves through exercise-induced adaptation. This is by no means an injunction to run through the pain but allow your body to heal and recover from the stress you put it under! Feed it properly, rest it properly, and let the cells in your bone recover appropriately.
This recovery will include adaptations that will reduce the likelihood of recurring shin splints.
Bonus Tips
While these are not scientifically proven ideas, I did want to share them because they are some things that have helped me in returning to running.
Bonus Tip #1: Run on an Incline
I am not entirely sure why this has helped but running at a 3% incline has seemed to stop shin splints from recurring even after extended breaks. My theory is that the increased loads your foot differently on impact and spreads the force out somewhat. Or perhaps increased dorsiflexion under load helps improve ankle mobility.
Bonus Tip #2: Neoprene Calf Sleeves
This was a recommendation that I was given years ago. There are a couple of reasons that this was supposedly helpful: the compression of the region helps prevent inflammation or the warmth of the neoprene helped the muscles stretch and be more flexible.
Bonus Tip #3: Proper Footwear
Individual variations in foot pronation and supination can make choosing the proper footwear essential. Some shoes are made for overpronation; someone with an oversupinated foot may develop pain or irregular movement patterns. Ensuring emphasis on ideal muscle balance and foot strength can help overcome either of these scenarios.
As always, if you or your client experiencing shin splints are having a difficult time recovering, refer to a qualified medical professional for treatment or reassessment.

References
Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments by Melanie Franklyn and Barry Oakes located at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4573502/